With the 2023 NIH Data Management and Sharing Policy going into effect on January 25, 2023, there’s no better time to explore data management resources! This post explores resources that can help you with your data management needs.
What is data management?
Data management involves the process of collecting or producing, cleaning and analyzing, preserving, and sharing data from a research project. Data management takes place throughout the entire research life cycle, from deciding on consistent file naming conventions to depositing the data in a repository for long-term archiving.
Why Data Management?
Data management is vital for transparency (showing your work promotes reproducibility of work), compliance (funding organizations and journals often require making data available), and personal and organizational benefit (using data within your own lab is easier with proper management).
I Think It’s FAIR to Say…
Understanding data management best practices is important to make well-informed decisions when selecting data management resources and tools. The FAIR Principles, first published in 2016, provide a set of guidelines for data management. FAIR stands for Findable, Accessible, Interoperable, and Reusable. You can learn more about the FAIR Principles on our Data Management Guide. Another great resource to help guide your data management is Cornell University’s Research Data Management Service Group’s Comprehensive Data Management Planning and Services Best Practices which provides extensive information related to best practices for:
Broad Data Management Resources
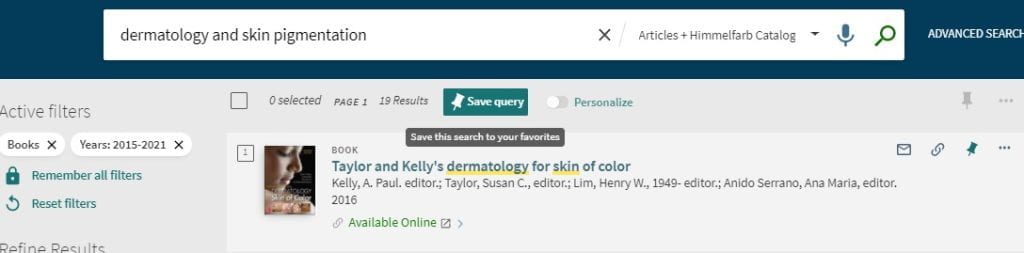
Himmelfarb’s Data Management Guide provides a wealth of information and resources related to data management. In addition to some basic information about data management, you’ll find information about NIH and NSF funder requirements. Data management plans (DMPs) are also covered in detail. The documentation and metadata page explains what metadata is, what should be included in your metadata, metadata schemas, controlled vocabularies, file naming conventions, and electronic lab notebooks. The data storage and security page includes data storage, storage formats, creating a backup plan, and data security. You’ll also learn about data sharing, including GW’s policy on regulated information, and data repositories.
I might need to make a plan for this…
Creating a data management plan (DMP) is often part of the grant writing process required by funding institutions. A comprehensive data management plan should address:
- Data Collection: Must be reliable and valid.
- Data Storage: Appropriate amount of data so research can be reproduced.
- Data Analysis: Interpretation of data from which conclusions can be derived.
- Data Protection: Ensuring sensitive data is safe and secure, preventing tampering or loss of data.
- Data Ownership: Addresses legal rights associated with data.
- Data Retention: Addresses how long data should be kept and proper disposal of sensitive data.
- Data Reporting: Publication of data.
- Data Sharing: Addresses what data can be shared with others and how.
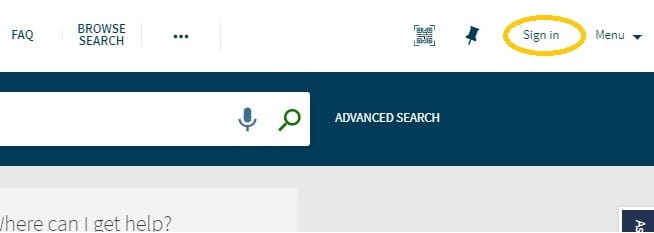
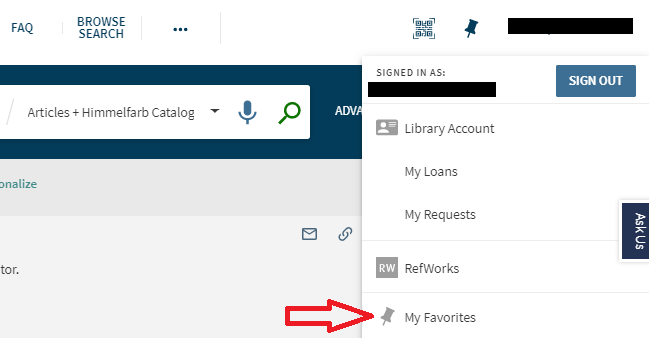
When it comes to creating a DMP, there are a number of tools available to help! The DMPTool is a free, open-source tool that helps researchers create DMPs that comply with funder requirements. DMPTool also provides links to funder websites, and best practices resources to help guide your data management efforts. Since GW is affiliated with DMPTool, GW users can create a personalized dashboard that allows them to see and organize the DMPs created through the tool. From the DMPTool’s website, simply click “sign in” and use Option 1 to search for George Washington University. Then log in with your GW UserID and password and create your data management plan!
The Framework for Creating a Data Management Plan, created by ICPSR, is a great outline that will help you create a DMP for your grant application. The framework includes a list of elements to be included, explains why each element is important and provides examples for each element. Michener’s article Ten Simple Rules for Creating a Good Data Management Plan is another great starting point to gain an understanding of the principles and practices of creating a DMP and ensuring your data are safe and shareable. For more DMP resources and to see examples and templates, check out the Data Management Plan page of the data management guide.
What’s Next?
Stay tuned for future posts on best practices for writing a data management plan, data storage, file naming conventions, creating “readme” metadata, and other data management topics. In the meantime, check out the lists of GW resources and additional resources below to learn more!
Additional GW Resources:
- Biostatistics & Epidemiology Consulting Service (BECS)
- Data Classification Guide (GW Office of Ethics, Compliance & Privacy)
- Data Protection Guide (GW Office of Ethics, Compliance & Privacy)
- CCAS Cloud Data Storage (GW Information Technology)
- GW Box (GW Information Technology)
- Backup, Storage, & Document Management (GW Information Technology)
- REDCap: Research Electronic Data Capture (GW SMHS)
Additional Data Management Resources:
- Biomedical Data Lifecycle (Harvard): Includes a Research Data Management Checklist.
- Borghi, J., Abrams, S., Lowenberg, D., Simms, S., & Chodacki, J. (2018). Support your data: A research data management guide for researchers. Research Ideas and Outcomes, 4, e26439.
- Introduction to the NIH Data Management and Sharing Plan (video)
- NIH Data Sharing: Coming 2023 (Virginia Commonwealth University guide)
- Understanding the New NIH Data Management and Sharing (DMS) Policy (video)