Background:
End-tidal CO2 monitoring is a measure of metabolism, perfusion, and ventilation - although we usually use it for the latter two.
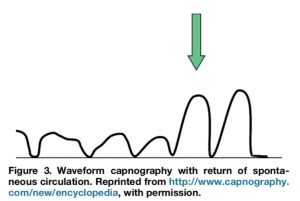
The waveform is really well-explained in this JEMS article, which is where this schematic is from. The main point is the EtCO2 number is at the peak of expiration.
EtCO2 in CPR
In 2014, two Norwegians published a great way to remember the uses of EtCO2 in CPR: PQRST. Look familiar? 😉 
Let's walk through these...
Position of the endotracheal tube (PQRST)
ACEP's policy is that direct visualization is great, and bilateral breath sounds are not reliable. As we know, we can't pause CPR to do a portable chest x-ray, which ACEP also notes is not reliable. They do recommend, however, ultrasound in the hands of an experienced operator and EtCO2.
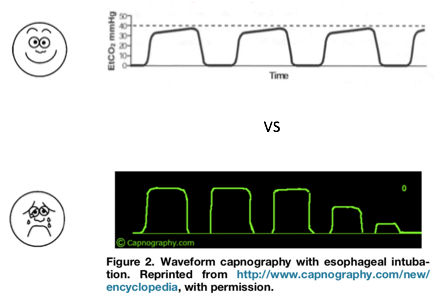
Waveform EtCO2 (vs. colorimetric) can be helpful because you may still get color change with the first few breaths of an esophageal intubation, which can be misleading. But the waveform does not lie (this schematic and the others were taken from this great JEM article).
Quality of CPR (PQRST)
We normally assess quality of CPR by palpable pulses (which can be challenging and even unreliable) or arterial diastolic pressure >25 (which is great if we have an arterial line). EtCO2 provides the same information in an objective, reliable way. We aim for EtCO2 of at least 10, with a goal of 20. (This is the official AHA guideline.) Why 10? CPR provides ~1/4 of normal cardiac output, and normal EtCO2 is 35-45.
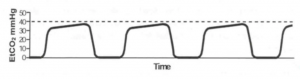
Return of spontaneous circulation (PQRST)
Getting ROSC can be detected on EtCO2 prior to a scheduled pulse check. An increase of EtCO2 to normal values (35-45) or an increase of 10 is 97% specific. (Unless you give bicarb right before, which artificially increases it.) (Source: this JEM article.)
Strategies for treatment (PQRST)
Different waveform morphologies can help us decide what our next steps should be.
For example, movement of a LUCAS device or ETT dislodgement:

Or the appearance of two smooshed EtCO2 waveforms, indicating a cuff leak, supraglottic intubation, or right mainstem intubation (basically, one part of the lungs ventilates before another):
Or, the waveform looks like a sharkfin, indicating expiratory obstruction (as in bronchospasm, kinked or blocked ETT or circuit):
Termination (PQRST)
Lastly, EtCO2 can provide one data point (of many) for when to terminate CPR. Chance of ROSC is significantly higher if EtCO2 >20 at 20 minutes, and significantly less if EtCO2 <10. (Also per the AHA guidelines.)
Caveats
I couldn't find much data on EtCO2 with bagged patients or patients with LMA's; using EtCO2 pretty much requires intubated patients. This is a touchy topic, as intubation can, as we know, decrease compression fraction by increasing time off the chest. There is also very little data on correlation of blood values of PCO2 vs EtCO2; animal studies do not show much correlation, and as you would expect with CPR, there will likely be some dead space and/or V/Q mismatch.
Take-home points
That said, there are some really great uses for EtCO2 in CPR: evaluating position of ETT, judging CPR quality, seeing ROSC quicker, adjusting strategies for treatment, and providing one data point for when to terminate resuscitation - some important things to keep in mind the next time your callbox goes off with a CPR in progress. Especially since it can be so quick to set up! (See video of me setting one up on an Alaris IV pump below).