EKG Contributor: Massoud Kazzi, MD
Resident Author: Jennifer Rabjohns, MD
Faculty Mentor: Massoud Kazzi, MD
Date of Presentation: 6/30/19
Introduction:
60yoF presents with syncope.
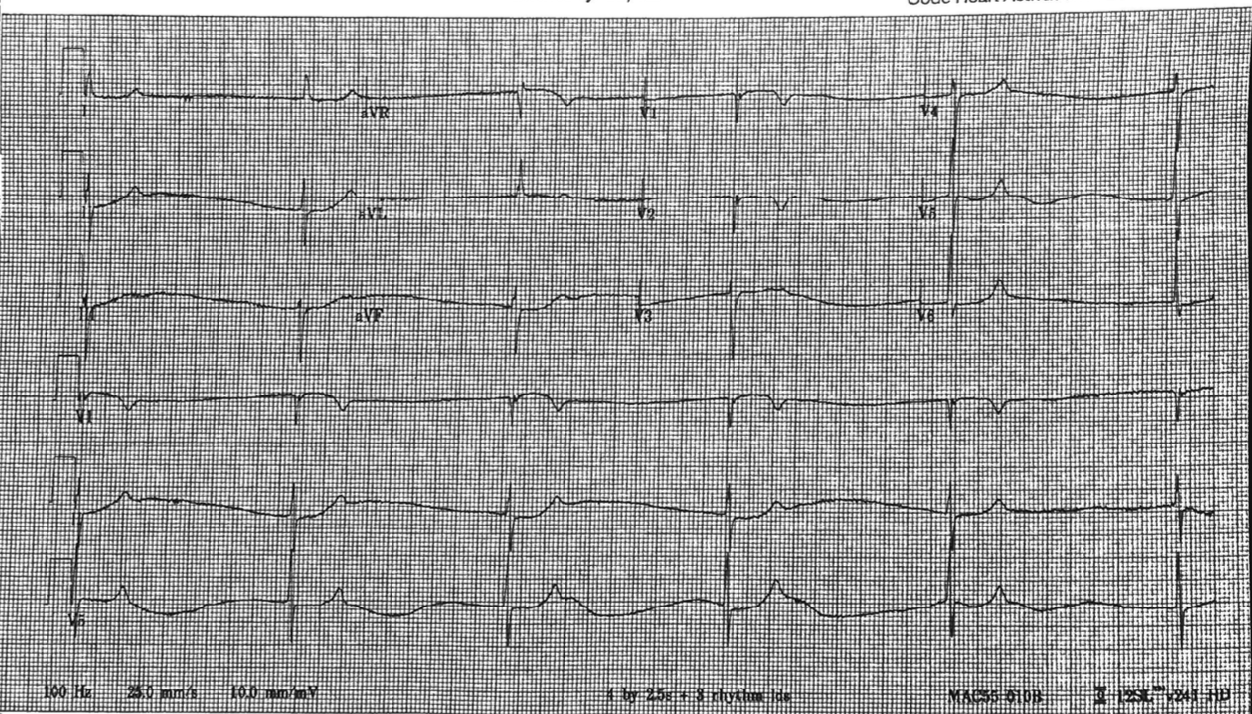
EKG is below:
How would you describe this EKG?
Narrow complex bradycardia without P waves. Rate is in the 20s, don't see P waves, but normal intervals. Peaked T's in the leads with tall R waves (V4-V6). No A-V blocks.
What is the differential diagnosis?
NEJM has a nice review article on bradycardia here. The list of causes is pretty long... (1).
On getting further history, this patient had a digoxin overdose.
Background:
Digoxin is a cardioactive steroid from the foxglove plant (2, 3).
Onset of action for oral digoxin is 1.5-6 hours; for intravenous, it's 5-30 minutes. It's cleared mostly renally, with some hepatic clearance.
Toxicity can be acute or chronic, and presents with gastrointestinal symptoms, altered mental status, the visual changes we've all seen on test questions (e.g., yellow halos around lights), and EKG changes (we'll review some below).
Antibiotics (especially macrolides), quinidine, verapamil, diltiazem, carvedilol, amiodarone, and spironolactone can all cause decreased digoxin protein binding to elevate digoxin levels up to two-fold.
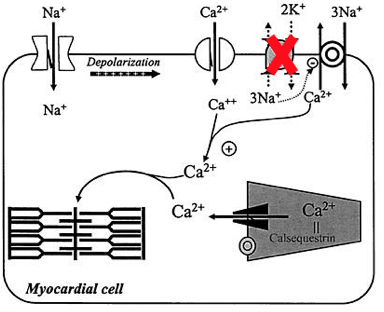
Hypokalemia enhances the effects of digoxin on the myocardium, possibly because digoxin doesn't have to compete with as much potassium - remember the mechanism of action here (2):
Digoxin causes increased intracellular Na -> increased intracellular Ca 2+ -> ionotropy.
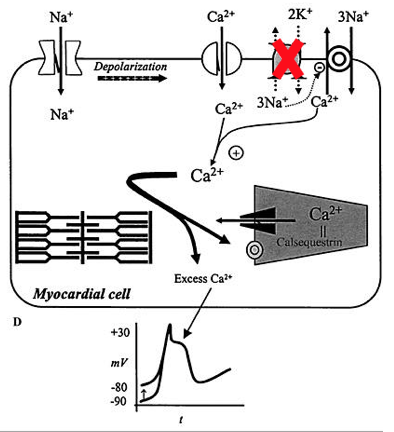
In toxicity, that high intracellular Ca 2+ -> higher resting membrane potential -> possible dysrhythmias and arrest.
Take-home points for digoxin toxicity (part 1):
- Toxicity can be acute or chronic. Look for presents GI symptoms, altered mental status, and visual changes (e.g., yellow halos).
- Antibiotics, calcium channel blockers, beta-blockers, amiodarone, and spironolactone decrease digoxin protein binding -> higher digoxin levels.
- Hypokalemia enhances effects of digoxin on myocardium.
- The elevated intracellular calcium in toxicity raises the resting membrane potential in the myocardium -> higher risk of spontaneous dysrhythmias.
References:
1. Mangrum, J. M., & Dimarco, J. P. (2000). The Evaluation and Management of Bradycardia. New England Journal of Medicine,342(10), 703-709. doi:10.1056/nejm200003093421006
2. Hack, J. B., & Lewin, N. A. (2006). Goldfrank's Toxicologic Emergencies(Vol. 8). New York, NY: McGraw-Hill. Retrieved June 26, 2019, from https://www.r2library.com/resource/detail/0071437630/ch0062s1649. Ch 62: Cardioactive Steroids
3. Foxglove: Toxic to the Heart. (n.d.). Retrieved June 26, 2019, from https://www.poison.org/articles/2015-mar/foxglove