If you haven’t heard by now, Urgent Matters holds an annual meeting at the American College of Emergency Physicians (ACEP) Scientific Assembly. While the exact theme changes from year to year, the meeting serves to bring together thought-leaders and innovators from the emergency medicine community. Thanks to Philips Blue Jay Consulting and Schumacher Clinical Partners, we are also able to acknowledge teams for developing and implementing effective solutions to common issues facing the emergency care community through our “Emergency Care Innovation of the Year Award.” This year, we received over 20 submissions and our reviewers narrowed them down to one winner and three honorable mentions.
Jesse Pines, MD MBA MSCE – Program Director, Urgent Matters
Rahul Sharma, MD MBA CPE – EM Physician-in-Chief & Medical Director, Strategic Initiatives
Hansen Hsu, MD – Director, EM Informatics & Co-Director, EM Telehealth Services
Peter Greenwald, MD MSC – Director, Telehealth QA & Co-Director, EM Telehealth Services
(Left to Right)
This year’s winner was New York Presbyterian/Weill Cornell Medical Center’s Emergency Department (ED) Telehealth Express Care Service. The ED Telehealth Express Care Service is an innovative ED-based telehealth program designed to streamline emergency care, reduce length of stay (LOS), and improve patient experience for patients with low acuity complaints.
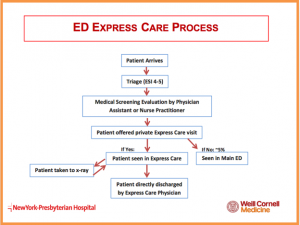
The process for ED Telehealth Express Care patients begin as it would for any other ED patient: an in-person triage and assessment. A registered nurse speaks with the patient and categorizes the severity of their medical complaint. Next, an Advanced Practice Provider (Physician Assistant or Nurse Practitioner) evaluates the patient, performs the Medical Screening Exam which is required for all ED visits, and decides whether the Telehealth program would be medically appropriate. Qualification for the Telehealth Express Care Service is based on set criteria (available in the UM Toolkit). Participation by the patient is voluntary. If the patient declines, a physician will examine them in-person. The telehealth encounter takes place with the on-call Telehealth Physician, a board certified Emergency Medicine faculty member. Evaluation, diagnosis, treatment, and education are discussed at-length, with family members present if desired. Discharge instructions are printed directly at the end of the visit by the physician with any prescribed medications sent electronically to a pharmacy of the patient's choice.
So, why would someone physically go to an emergency department, only to be seen by a remote physician through a screen? Dr. Sharma responds in an Urgent Matters podcast:
“When was the last time you actually went to the bank and went to the teller instead of the ATM to get cash? You don’t, you only go in when you need a certified check or something complicated.”
The data supports him. The ED Express Care Service has been in place since July 2016 is available at two of six EDs at New York Presbyterian: Weill Cornell - a Level 1 Trauma Center, and Lower Manhattan - a community hospital. Together these hospitals see an annual volume of over 140,000 visits. To date, over 4,000 patients have been through the ED Express Care Service with impressive results. Express Care Service has helped reduce wait times for low-acuity patients from 2.5 hours to an average 39 minutes from arrival to discharge. The project also helps to establish primary care appointments, and twenty percent of patients receive follow-up appointments via the in-house ED patient navigator program with a primary care physician or sub-specialist prior to discharge. From the first year of data, Express Care patients, compared to those receiving a traditional fast track evaluation, were younger (median age: 38 [IQR, 27-54] vs. 43 [31-58]; P<0.001) and more likely to be male (52% vs. 46%; P<0.001), Express Care patients had less acute illness as measured by triage severity score (ESI 4 or 5: 97% vs. 84%; P<0.001), and more likely being treated for wound check/suture removal and infectious illness. Express Care patients were less likely to have x-rays preformed as part of their ED evaluation (24% vs. 42%; P<0.001). Express Care patients were treated and released more quickly than fast track patients (median time door to discharge 39 minutes as compared to 120 minute). Express Care patients were less likely to return within 72 hours, and no Express Care patient returning within 72 hours required admission to the hospital. There was a trend to higher Press Ganey satisfaction among Express care patients as compared to fast track ED patients (median: 100 [87-100] vs. 89 [74-100]; P=0.15). Another analysis listed in their submission comparing older patients to younger patients in express care found that although Express Care patients trended younger than traditional ED pathway patients on average, patients 60 and older comprised 24% of the total Express Care population, indistinguishable from the percentage of people 60 and older in the conventional treatment fast track area. Among patients 60 years and over seen in Express Care, the average age was 72. There were no significant differences by age group with respect to 72 hour returns to the ED and a low likelihood for a change in treatment plan on return. In addition to eliciting patient feedback regarding satisfaction with the ED experience, the team surveyed participating physicians about their telemedicine background and experience with the program, with most physicians reporting a significant increase in comfort and positivity about telemedicine patient encounters. Future Direction
Future Direction
At the Urgent Matters meeting, Dr.’s Rahul Sharma, Peter Greenwald, and Hanson Hsu spoke on plans to expand the project by incorporating nursing homes consultation, telehealth kiosks in NYC pharmacies, and paramedic telemedicine visits for CHF patients. Dr. Greenwald also briefly mentioned the value of engaging with insurance companies to provide coverage for virtual urgent care as part of a benefits package. Dr. Ali Raja, Vice Chairman of the Department of Emergency Medicine at Massachusetts General Hospital was quoted in the Wall Street Journal saying, “Ten years from now, tele-emergency medicine will be the standard around the country. We’ll still have emergency departments for those patients who are critically ill, but I think we’re all headed in this direction.”
Personally, I would like to extend my congratulations to the ED Express Care team for their innovative, patient-centered, and value-driven work. Make sure to look out for an upcoming webinar with the New York Presbyterian/Weill Cornell Medical Center team (subscribe here).
For more:
- Urgent Matters Toolkit Submission
- NYP On-Demand
- ACEP Now
- Crain’s Health Pulse
- The Wall Street Journal
- New England Journal of Medicine Catalyst.
Ameer Khalek is a MPH student at the GWU Milken Institute School of Public Health