Objectives
- Identify histological features of the following viscera: ovaries, uterine tubes, uterus, cervix, and vaginal canal
- Review histologic features of the urethra (also explained in the urinary system section)
- Identify histologic features of the external genitalia (depending on your course, check with your session lead)
- Identify histologic features of the placenta
Overview
Disclaimer: The following information describes anatomical features a reproductive system in which an individual is genetically XX with no atypical variation or surgical intervention and contains the above listed viscera. The term “female” will be used to refer to this collection of viscera.
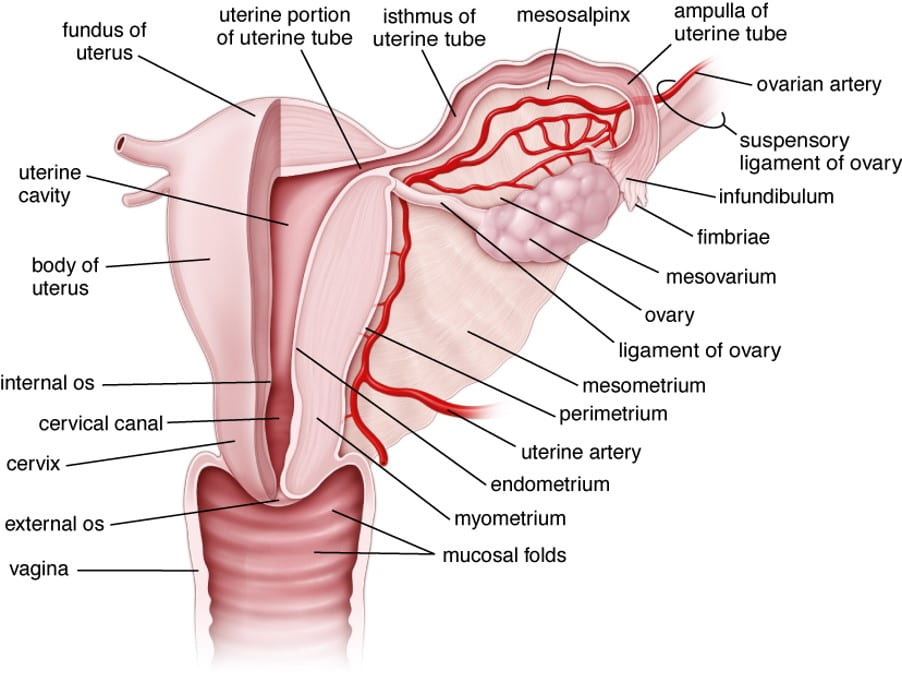
The female reproductive organs generally described below include the ovaries, uterine tubes, uterus and cervix, and vaginal canal including the urethra and external genitalia which are closely related to the organs of reproductive function and development. Below is an overview of the internal and external viscera.
Internal Reproductive Viscera:
- Ovaries: produce hormones and prepare oocytes for fertilization. Almond-shaped, made up of a cortex and medulla. The ovary surface is covered by germinal epithelium (simple cuboidal-squamous) and the tunica albuginea (dense CT), between the germinal epithelium and the cortex. The cortex contains developing follicles and the medulla contains loose CT with blood vessels, lymphatic vessels and nerves. More details on the stages of follicles and post-ovulation structures are found below with the specimen slides.
- Uterine tubes: extend from the uterus to the ovaries and provide passage to the uterus. The tubes are grossly divided into 4 parts: 1) distally is the infundibulum (funnel-shaped) with fimbriae (finger-like projections); 2) ampulla– longest segment, site of fertilization; 3) isthmus– narrow, close to uterus; 4) uterine/intramural part- lies within the uterine wall. Layers of the tubes: mucosa– simple columnar epithelium with ciliated cells and secretory peg cells; there is no submucosa; muscularis– inner circular and outer longitudinal with no distinct boundary; serosa– mesothelial cells and CT.
- Uterus: consists of the body and cervix (described separately below). Layers of the uterine wall include: endometrium (mucosa), myometrium– (smooth muscle), and perimetrium.
- Endometrium- undergoes cyclic changes each month. Consists of 2 zones: stratum functionale (lost during menstruation) and stratum basale. Simple columnar epithelium with a mix of ciliated and secretory cells invaginates into the lamina propria, glands develop during cycle, more details can be found below with the specimen slide. Blood supply: Radial arteries are found in the stratum basale and becomes spiralized (spiral artery) as it extends into the stratum functionale. Radial arteries give off smaller straight arteries which supply the endometrium. The most distal arteries develop large lake-like structures known as lacunae in the stratum functionale.
- Myometrium- 3 indistinct layers of smooth muscle, stratum vasculare (large blood vessels and lymphatics); growth during pregnancy is mainly due to hypertrophy of existing smooth muscle cells extending from about 50μm to >500μm.
- Perimetrium- anterior adventitia, posterior serosa/peritoneum.
- Cervix: inferior 1/3 of the uterus forming a canal that leads from the internal os to the external os, ending in the vagina. Mucosa– contains branched cervical glands which undergo functional changes in relation to the menstrual cycle, lacks spiral arteries, little change in thickness during menstrual cycle (no shedding), epithelium transitions from simple columnar in the cervical canal (endocervix) to stratified squamous in the vaginal part (ectocervix). Cervical wall– dense CT with little muscle fibers.
- Vagina: a fibromuscular tube extending from the cervix to the vestibule. Mucosa– stratified squamous epithelium, non-keratinized, lacks glands + lamina propria with papillae that extend into the epithelium. Muscular layer– 2 indistinct layers of smooth muscle with some skeletal muscle fibers (bulbospongiosus). Adventitia– inner dense CT layer and outer loose CT layer that blends into surrounding tissue with numerous blood and lymphatic vessels and nerves.
- Urethra: short tube with transitional epithelium that changes to stratified squamous epithelium distally. Muscle fibers of the external urethral sphincter can be found where the urethra traverses the urogenital diaphragm. Empties into the vestibule of the vagina.
External Viscera:
- Mons pubis and Labia majora– skin with hair follicles covers subcutaneous adipose tissue. The labia majora contain a thin layer of smooth muscle, similar to the dartos muscle of the scrotum. They also contain nerve endings including Meissner’s corpuscles, Pacinian corpuscles and free nerve endings. The inner surface of the labia majora lack hair follicles. Sebaceous and sweat glands are present.
- Labia minora– thin folds of hairless skin with abundant melanin pigment. Lack of fat in the center CT but there are numerous blood vessels, elastic fibers and sebaceous glands.
- Clitoris– an erectile structure homologous to the penis. Consists of erectile bodies, the corpora cavernosa, that extend from the pelvic bone (pubic rami) anterior and just superior to the vestibule of the vagina where they join as the glans clitoris which contains numerous nerve endings. It is covered by a hood of skin known as the prepuce from the labia minora.
- Vestibule, including lesser and greater vestibular glands– the vestibule is the space between the two labia minora which contains the openings for the vaginal canal, urethra, and ducts from the lesser and greater vestibular glands. The lesser vestibular glands (Skene glands) are found on either side of the external urethral orifice. They function to help lubricate the vaginal canal during arousal. The greater vestibular (Bartholin’s) glans are found at the base of the vestibular bulbs (corpora spongiosa erectile tissue) and empty into the vestibule. These tubuloalveolar glands secrete mucous for lubrication.
Placenta:

The placenta forms from both maternal (decidua basils) and fetal (chorion) tissues. It undergoes drastic structural changes as it is forming and serves as the site of nutrient and waste exchange. Here, we are focusing on a fully-formed placenta. The unbiblical cord contains the vessels that bring nutrients to the fetus. The umbilical vein brings oxygen and nutrient-rich blood from the placenta to the fetus. Once that blood moves through fetal circulation, the deoxygenated and nutrient-poor blood returns to the placenta through the two umbilical arteries. Structures:
- Cotyledons– 15-20 wedges divided by decidual septa of dense CT
- Villi– branched projections of fetal chorion that extend into lacunae where nutrient exchange takes place. Villi consists of: simple cuboidal epithelium made of cytotrophoblasts (early pregnancy) and synctiotrophoblasts (clusters form syncytial knots); and stroma with capillaries, venules mesenchymal cells, reticular cells, fibroblasts, myofibroblasts, smooth muscle, and fetal placental antigen-presenting cells (macrophages, historically known as Hofbrauer cells).
- Placental arteries bring maternal blood to lacunae
- Basal plate (stratum basalis)- maternal portion of placenta which anchors some villi and contains decidual cells (help with implantation and produce relaxin).
Internal Reproductive Viscera + Placenta Slides

In this specimen of the ovary, you will first start by identifying the cortex and medulla. When analyzing the cortex, identify the tunica albuginea (dense CT) and germinal epithelium (simple cuboidal and simple squamous). Examine the medulla where you will find neurovasculature of the ovary. Deeper in the cortex you will find follicles in different stages:
- Primordial follicles– 30μm in diameter, found close to the tunica albuginea consisting of a single layer of squamous follicle cells surrounding an oocyte. In high resolution images, you can identify the Balbiani body, collection of the organelles in the oocyte cytoplasm.
- Primary follicles– at first, simple cuboidal follicular cells surrounding an oocyte (unilaminar). Development of the zona pellucida– pink ring between the cuboidal cells and oocyte. Simple cuboidal epithelium becomes stratified cuboidal and the follicle cells are now granulosa cells (with microvilli) (multilaminar). The stratified cell layer is now known as the stratum granulosum and becomes surrounded by connective tissue known as theca folliculi (theca interna and theca externa).
- Secondary follicles– found deeper in the cortical stroma and characterized by the beginning formation of fluid-filled cavities among the granulosa cells eventually forming a single antrum. The cumulus oophorus also appears during this stage, projecting into the antrum. Cells of the cumulus oophorus immediately surrounding the oocyte are known as the corona radiata.
- Mature (Graafian) follicles– ≥10 mm, the stratum granulosum becomes thinner as the antrum grows in size and the thecal layers become more prominent. The oocyte and cumulus cells begin to loosen from the rest of the granulosa cells. Due to the size, you may not see the oocyte in the section.
- Antral follicles– most ovarian follicles do not undergo complete maturation and become atretic at any stage of maturation. You will see signs of degeneration such as shrinkage of cells and loss of structure.
In the right bottom corner of the slide, there is a portion of the neurovasculature bundle that travels through the suspensory ligament.
Check out the “More Practice” section to practice identifying follicles of different stages.

After ovulation events, ovaries take on new structures left from the ovulation event and cells that were once part of the mature follicle. The corpus luteum is a temporary endocrine organ that forms just after ovulation of the oocyte and is composed of 2 cells types: 1) granulosa lutein cells (large, eosinophilic cytoplasm) that secrete progesterone and convert androgens into estrogen; and 2) theca lutein cells more peripherally located, smaller cells that secrete androgens and progesterone. At first, the corpus luteum appears as to have a central clot of blood and is known as the corpus hemorrhagicum. The general function of the corpus luteum is to support the developing embryo if fertilization takes place until the placenta is established. The corpus luteum eventually degenerates into a scar known as the corpus albicans and shrinks over time. Use this slide to look for a corpus luteum and corpus albicans.

In this specimen of the uterine tube, start with the lumen and work through the layers of the uterine tube to identify cells and structures. The most inner layer is the mucosa, identify the simple columnar epithelium and look for the ciliated and secretory peg cells. Notice the mucosal folds that project into the lumen. Examine the muscularis externa layer for smooth muscle cell directions. Examine the serosa and you may find some mesothelial cells. The mucosa layer undergoes some changes throughout the length of the tube. The folds are more numerous and complex in the ampulla but become smaller and more simple as you move towards the isthmus.

In this specimen, you can identify the 3 layers of the uterus: endometrium, myometrium, and perimetrium. Take a close look at the endometrium of this proliferative uterus. Notice the shape of the glands in the stratum functionale that extend from the basale. They have narrow lumina and are relatively straight. During this time, stromal cells are proliferating while secreting collagen and ground substance. The spiral arteries are lengthening. At the end of this phase, the endometrium is about 3mm thick and the basal portion of the epithelial cells appear lighter in stain due to the accumulation of glycogen (not in this specimen as it is not at the end of the proliferative phase). When examining the myometrium, notice you will see a random arrangement of smooth muscle in both cross-section and longitudinal section. As you look through the slide, review the vasculature you would see in each layer. The most outer layer of cells of the perimetrium are not clear enough to determine if this is from the anterior adventitia or posterior serosa portion of the uterus.

In this specimen slide, pay close attention to the appearance of the uterine glands in comparison with the previous slide. Take a look at the lamina propria, you will see there are different cell types present including lymphocytes and macrophages. Review the vasculature of the uterus.

This specimen is taken from 1 side, remember the entire cervix includes a cervical canal leading to the external os which opens into the vaginal cavity. Using this specimen of the cervix, use the epithelium to determine the location of the endocervix (simple columnar) and ectocervix (stratified squamous). Once you have found the endocervix, you will have located the placement of the lumen of the cervical canal. Notice there are numerous cervical glands in the endocervix but very few in the ectocervix, especially moving laterally into the vaginal space. You will also notice there is less smooth muscle in comparison with the uterus in the stroma.

When examining the specimen of the vaginal wall, notice the epithelium is similar to that of the ectocervix. The lamina propria projects into the epithelium creating papillae. Look for bands of smooth muscle in the muscularis layer. As you move through the slide, identify the urethra and review the epithelium of that structure.

When looking at the placenta, first identify the amnion and chorionic plate (fetal side) then the basal plate (endometrial side). The amnion consists of simple cuboidal epithelium resting on connective tissue and the chorion is filled with fibrous connective tissue. The basal plate consists of embryonic tissues (trophoblast- thin layer of syncytiotrophoblast + cytotrophoblast) and maternal tissue. Within the basal plate, you should see the collections of large decidual cells. This is a full-term, mature placenta. Take a close look at the tertiary villi surrounded by an incomplete layer of cytotrophoblast cells and a complete layer of syncytiotrophoblast cells. You will also see some syncytial knots, indicative of a full-term placenta.
External Viscera

The labia minora are covered with skin, stratified squamous lightly keratinized epithelium. Notice there are no hair follicles but you do see several sebaceous glands present. There is little to no fat found in the dermis of the labia minora but you will see numerous bundles of smooth muscle and nerves which can look similar. Remember that peripheral nerves are encapsulated.

This is a section of the glans clitoris. It is surrounded by dense connective tissue, tunica albuginia, which extends to separate the 2 erectile tissues, corpora cavernosa, in an incomplete septum. The corpora cavernosa tissue is filled with vascular spaces created by smooth muscle trabeculae. There are also numerous vessels and nerves.
External Viscera Answers
Slide Labia Minora
- A) black- stratified squamous, keratinized; B) red- keratinized cells (no nuclei); C) green- sebaceous glands
- Meissner corpuscle (free nerve ending)
- Area of interest, no questions
Slide Clitoris
- Orientation, no questions
- A) black- artery; B) blue- vein; C) green- nerve; notice there are lots of neurovascular bundles
- Smooth muscle
- Blood
- Tunica albuginea
More Practice
Use the digital specimens slide below to practice identifying different viscera and histologic features of these viscera including stages of follicles and tissue types in each organ. Answers are in the section below.








Use the above specimen slides to identify which uterus is in the proliferative phase, secretory phase, and menstrual phase. Open each slide to examine the epithelium. Slide A and B sections allow you to see the full lumen of the uterus while slide C is just a portion of one side of the lumen. Links to each slide:
More Practice Answers
Slide Michigan 239 Ovary
- Orientation, no questions
- A) black- germinal epithelium, simple cuboidal to squamous; B) black- tunica albicans, dense irregular CT
- A) green- primary follicles (the one to the left is unilaminar, one on the right is multilaminar); B) blue- primordial follicles; C) white- zona pellucida
- A) Secondary follicle; B) green- corona radiata; C) blue- cumulus oophorus; D) red- stratum granulosum, convert androgen to estrogen; E) yellow- theca folliculi
Slide GWU 85 Ovary
- A) black- germinal epithelium (simple cuboidal); B) green- tunica albuginea
- Corpus albicans
- A) black- theca lutein; green- granulosa lutein
- A) black- primary, unilaminar; B) blue- primordial; C) green- primary, multilaminar
Slide GWU 75
- A) vagina; B) black- stratified squamous non-keratinized, glycogen storage; C) blue- urethra, transitional epithelium or urothelium (blue arrows point to umbrella cells)
Slide GWU 74
- A) this is the cervix; B) black- ectocervix; C) green- endocervix
Slide Iowa Ovary and Uterine tube
- A) black- ovary; B) blue- fimbriae of uterine tube; C) green- different section of uterine tube
- A) white- primordial; B) black- primary, unilaminar
- A) Primary, multilaminar; B) zona pellucida
- A) mature follicle; B) blue- theca folliculi; C) yellow- stratum granulosum cells
- Simple columnar, ciliated
- Smooth muscle
Slides Uterus (3)
- A. Secretory- notice the dilated, saw-tooth glands
- B. Proliferative- the glands are very straight and narrow
- C. Menstrual- the epithelium is loosing structure
